Glaucoma: Things You Need To Know
Key Highlights
- Glaucoma leads to vision loss
- Caffeine increases your risk of developing glaucoma
- Fruits and vegetables fight glaucoma
- Glaucoma can be managed even without surgery
The eyes are the window to the world. This famous saying could not be more relatable. Your eyes are those organs in your body that allow you to see. They take up the light from your surroundings and use it to send information to your brain. They are a natural magical set of gifts!
Your eyes can see about 200 degrees in all directions, including in front of you and to the sides. Different parts of your eyes work together to allow you to see images, movement, and depth. Your eyes can see millions of colors in varying shades. However, many conditions can affect the way your eyes work. These include common vision problems like myopia (nearsightedness), astigmatism, and eye injuries. Some diseases may not be eye-related but can still cause problems in your eyes like diabetes and high blood pressure.
What is glaucoma?
Glaucoma is a group of eye conditions that damage the optic nerve, the health of which is vital for good vision. This damage is often caused by abnormally high pressure in your eye. In most cases, fluid builds up in the front part of the eye. This extra fluid puts pressure on the eye, gradually damaging the optic nerve. This pressure is known as intraocular pressure (IOP), or eye pressure.
Glaucoma is one of the leading causes of blindness for people over the age of 60 and the second leading cause of blindness globally. Globally, it is estimated that 5.7 million people are visually impaired as a result of glaucoma. It can occur at any age but is more common in older adults. Untreated or poorly controlled glaucoma can lead to permanent and irreversible vision loss and blindness.
1. Does glaucoma have many sides to it? Types of glaucoma
There are different types of glaucoma listed below:
Open-angle glaucoma: It is the most common form of the disease. The drainage angle formed by the cornea and iris remains open, but the trabecular meshwork is partially blocked. This causes pressure in the eye to gradually increase and this damages the optic nerve. This process is so gradual that you will barely notice a problem in your eyes.
Closed-angle glaucoma: Also known as closed-angle glaucoma, this condition occurs when the iris bulges forward to narrow or block the drainage angle formed by the cornea and iris, resulting in a fluid that cannot circulate through the eye and thus puts pressure on the eye. This condition may occur suddenly or gradually. Acute angle-closure glaucoma is a medical emergency.
Normal-tension glaucoma: In this condition, your optic nerve becomes damaged even though your eye pressure is within the normal range. No one knows the exact reason for this. You may have a sensitive optic nerve, or you may have less blood being supplied to your optic nerve. This limited blood flow could be caused by atherosclerosis — the buildup of fatty deposits (plaque) in the arteries or other conditions that impair circulation.
Glaucoma in children: Infants and children can have glaucoma. It may be present from birth or develop in the first few years of life. The optic nerve damage may be caused by drainage blockages or an underlying medical condition.
Pigmentary glaucoma: In this condition, pigment granules from your iris build up in the drainage channels, slowing or blocking fluid exiting your eye. Activities such as jogging sometimes stir up the pigment granules, depositing them on the trabecular meshwork and causing intermittent pressure elevations.
2. What can give rise to glaucoma?
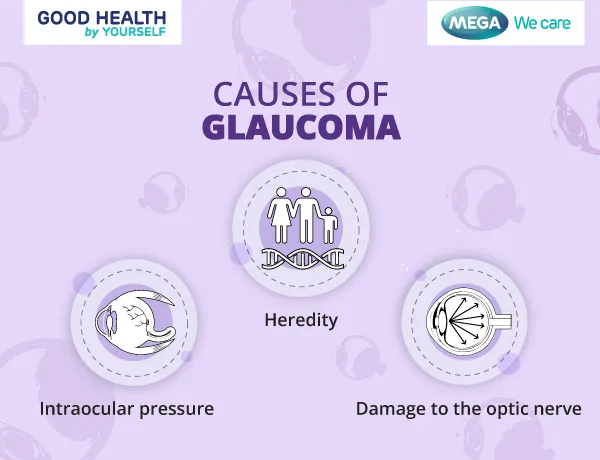 Glaucoma can occur without any cause however, several factors tend to give rise to it.
Glaucoma can occur without any cause however, several factors tend to give rise to it.
Intraocular pressure: This is the most common cause of glaucoma. Your eyes produce a fluid called aqueous humor that nourishes them. This liquid flows through the pupil to the front of the eye. In a healthy eye, the fluid leaves through a drainage canal located between the iris and cornea. With glaucoma, the drainage canals become clogged with microscopic deposits. The fluid has nowhere to go, so it builds up in the eye and puts pressure on it.
Damage to the optic nerve: Glaucoma can also result from damage to the optic nerve. As this nerve gradually deteriorates, blind spots develop in your visual field. For reasons that doctors don't fully understand, this nerve damage is usually related to increased pressure in the eye.
Heredity: Glaucoma tends to run in families. In some people, scientists have identified genes related to high eye pressure and optic nerve damage.
3. What are the risk factors associated with glaucoma?
 Glaucoma can lead to vision loss. Thus, it is important to be aware of the risk factors associated with this disease, such as:
Glaucoma can lead to vision loss. Thus, it is important to be aware of the risk factors associated with this disease, such as:
Health status: Your body physiology and health status may influence the occurrence of glaucoma like having high intraocular pressure, being over the age of 60 years, having corneas that are thin at the center, and being extremely near-sighted or far-sighted.
Race: Being black, Asian, or Hispanic.
Heredity: Having a family history of glaucoma.
Pre-existing medical conditions: Having certain medical conditions, such as diabetes, heart disease, high blood pressure, and sickle cell anemia.
Eye damage: Having had an eye injury or certain types of eye surgery.
Medications: Taking corticosteroid medications, especially eyedrops, for a long time.
4. How will I know if I have developed glaucoma? Signs and symptoms related to glaucoma
Signs of open-angle glaucoma tend to come on subtlety and gradually, making it difficult for people to notice them. However, these symptoms may be noticed,
- Patchy blind spots in your side (peripheral) or central vision, frequently in both eyes
- Tunnel vision in the advanced stages
Closed-angle glaucoma has more severe symptoms that tend to come on suddenly. These include,
- Severe headache
- Eye pain
- Nausea and vomiting
- Blurred vision
- Halos around lights
- Eye redness
More or less any type of glaucoma is accompanied by eye pain and pressure, headache, rainbow-colored halos seen around the lights, blurred vision, red eyes, and nausea and vomiting.
What are the next steps on being diagnosed with glaucoma?
It's quite possible that you have glaucoma and do not know it. Regular eye exams may help you assess your optic health. To check for glaucoma, your eye doctor may do one or more of these painless tests:
- Dilated eye exam to widen pupils and view the optic nerve at the back of the eyes.
- Gonioscopy to examine the angle where the iris and cornea meet.
- Optical coherence tomography (OCT) to look for changes in the optic nerve that may indicate glaucoma.
- Ocular pressure test (tonometry) to measure eye pressure.
- Pachymetry to measure corneal thickness.
- Slit-lamp exam to examine the inside of the eye with a special microscope called a slit lamp.
- Visual acuity test (eye charts) to check for vision loss.
- Visual field test (perimetry) to check for changes in peripheral vision (your ability to see things off to the side).
Treatment of glaucoma
If left untreated or neglected, glaucoma can aid in faster and permanent vision loss, making you blind. Glaucoma treatments can slow down vision loss, but they can't restore lost vision. It's important to see your eye doctor right away if you have eye pain, severe headaches, or vision problems. Usually, it is the chronic form of open-angle glaucoma that responds well to medical or pharmacological intervention. First-line treatment options are considered to be either topical beta-blockers, e.g. timolol; or prostaglandin analogs, e.g. latanoprost. Various treatments available for glaucoma are listed below;
1. Nonpharmacological measures:
Surgical intervention using an iridectomy provides the most definitive treatment option in patients with closed-angle glaucoma. This procedure may also be performed using a surgical laser and creates an opening in the iris through which the aqueous humor is allowed to drain more freely in a severely congested, hypertensive eye. Surgery can help slow down vision loss, but it can't restore lost vision or cure glaucoma.
2. Pharmacological measures:
Currently, the mainstay of glaucoma treatment is lowering the IOP. There are several different classes of available IOP-lowering agents, namely:
- Alpha-adrenergic agonists, e.g. apraclonidine and brimonidine.
- Beta-blockers, e.g. betaxolol, levobunolol and timolol.
- Carbonic anhydrase inhibitors, e.g. acetazolamide and dorzolamide.
- Cholinergic agonists, e.g. carbachol and pilocarpine.
- Prostaglandin analogues, e.g. latanoprost and travoprost
Prescription eyedrops containing the various classes of medicines, decrease fluids and increase drainage to alleviate eye pressure.
What can be done to avoid this disease?
Regular eye examination: Early detection of glaucoma through routine eye exams is the best way to protect eye health and prevent vision loss. Glaucoma testing should occur every:
- 1 to 2 years after age 35 for people at high risk.
- 2 to 4 years before age 40.
- 1 to 3 years between ages 40 and 54.
- 1 to 2 years between ages 55 to 64.
- 6 months to 12 months after age 65.
Know your family history: Glaucoma tends to run in families. If you're at increased risk, you may need more frequent screening.
Exercise safely: Regular, moderate exercise may help prevent glaucoma by reducing eye pressure. Talk with your doctor about an appropriate exercise program.
Using prescription eyedrops regularly: Glaucoma eyedrops can significantly reduce the risk that high eye pressure will progress to glaucoma. To be effective, eyedrops prescribed by your doctor need to be used regularly even if you have no symptoms.
Wear eye protection: Serious eye injuries can lead to glaucoma. Wear eye protection when using power tools or playing high-speed racket sports in enclosed courts.
Role of food in glaucoma
A common question, patients with (or at risk for) glaucoma ask their ophthalmologist is, what can they do by themselves next to just taking their daily ophthalmic medication? Patients often look for alternatives. Several studies have suggested that nutrition might affect IOP or glaucoma. Nutrition may affect glaucomatous eyes through their antioxidative properties, their effect on the blood flow/vascular endothelium, or their neuroprotective properties.
The use of complementary and alternative medicine (CAM), targeting both IOP-dependent and non-IOP-dependent mechanisms, in glaucoma has received interest from some ophthalmologists. A major domain of CAM in glaucoma is the utilization of dietary interventions. Research suggests that an individual's diet may affect IOP, the incidence of glaucoma, and the progression of the disease.
Here's how different kinds of food impact your chances of getting glaucoma:
- Alcohol - It has been shown that alcohol lowers IOP following acute ingestion.
- Coffee - Coffee is a rich source of caffeine. A transient elevation in IOP has been noted following caffeine ingestion in patients with different types of glaucoma.
- Tea - Flavonoids, a major polyphenol in tea, are thought to play a role in glaucoma, they reduce oxidative stress and improve blood flow.
- Ginkgo biloba extract (GBE) - increases ocular blood flow, improves retinal ganglion cell survival, and protects against oxidative stress.
- Fruits and vegetables - Being rich in antioxidants, it is speculated that a diet rich in fruits and vegetables can decrease the risk of developing glaucoma. The research concluded that there is a decreased likelihood of glaucoma among women that reported a greater intake of fruits and vegetables rich in vitamins A and C, and carotenes.
It is hypothesized that high consumption of dietary nitrates might have a protective effect against the development of primary open-angle glaucoma. Selenium and iron may increase the risk of glaucoma, glutathione plays an important role in regulating oxidative stress in eyes with glaucoma and nitric oxide (especially dark green leafy vegetables containing high nitrate) seems to have a beneficial effect on glaucoma.
1. What not to eat in this disease? Foods to avoid in glaucoma
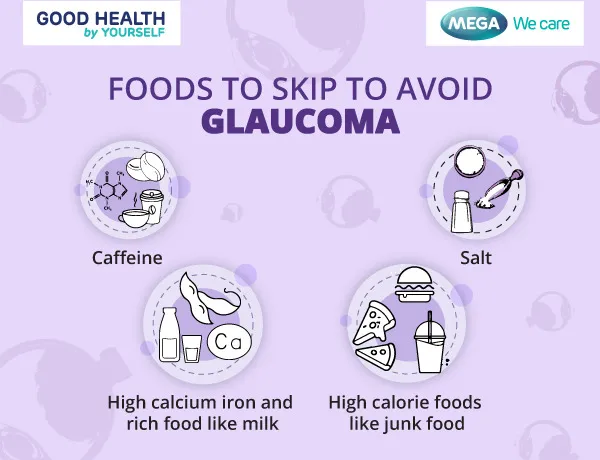 Caffeine may transiently elevate IOP by either promoting aqueous production or inhibiting the outflow facility. It may thus increase the risk of developing glaucoma.
Caffeine may transiently elevate IOP by either promoting aqueous production or inhibiting the outflow facility. It may thus increase the risk of developing glaucoma.
Oxidative stress has been suggested to play a role in glaucoma pathogenesis. As oxidants, calcium and iron have been implicated to impact the function of trabecular meshwork and retinal ganglion cells in glaucoma subjects.
Frequent salt intake may also contribute to open-angle glaucoma. High-calorie diets (restricting fat) may also increase the development of glaucoma.
A glaucoma prevention diet should thus avoid excess caffeine, high calcium and iron, excess salt, and high calories.
2. What to eat in this disease? Diet for glaucoma
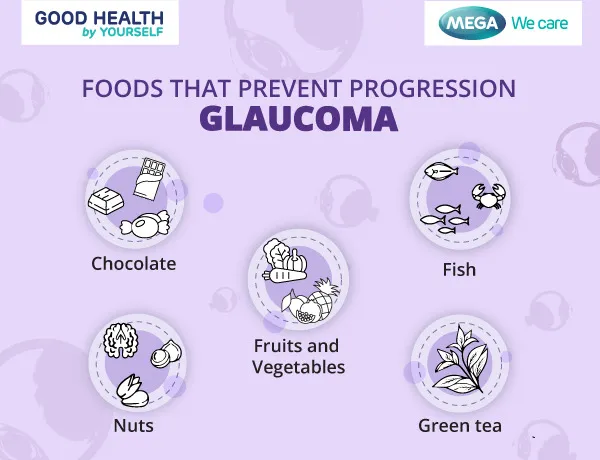 Based on the various effects of different kinds of foods, it is best to, consume abundant amounts of fruits and vegetables (carrots, green leafy vegetables), fish and nuts, rich in polyunsaturated fatty acids, and careful consumption of red wine, chocolate, and green tea to help prevent the further progression or development of glaucoma.
Based on the various effects of different kinds of foods, it is best to, consume abundant amounts of fruits and vegetables (carrots, green leafy vegetables), fish and nuts, rich in polyunsaturated fatty acids, and careful consumption of red wine, chocolate, and green tea to help prevent the further progression or development of glaucoma.
How can I live better with glaucoma
If you are one of those diagnosed with glaucoma, it's important to know that you can take steps to slow or prevent its progression, especially if it is detected early. Here are a few tips to live better with glaucoma;
- Adhere to medications - Maintain a schedule to take the proper dosage on time. Set alarms and alerts on devices you keep close, such as your cellphone, watch computer, or tablet for reminders.
- Avoid falls and accidents - Glaucoma may increase the risk of falling and accidents due to loss of side vision. It is important to mark boundaries in your home. Areas such as doorways, drawers, counters, and table edges can be identified with bright or contrasting colored tape or paint.
- Maintain a healthy lifestyle - Exercise can improve the health of the eye as well as the rest of your body.
- Look for support - Seek help from friends and family for transportation and other means of support. A support team can help with many of the above tips, including medication management and healthy habits.
Conclusion
Glaucoma is a devastating disease to be diagnosed with, especially since it can lead to irreversible vision loss. It is a very common eye disorder that impacts millions of people worldwide. However, it can be managed with the correct therapy and support, when received on time.
Glaucoma can be treated with medicines as well as surgical methods. You can also follow lifestyle changes like exercise, and dietary changes like the incorporation of green leafy vegetables, fruits, fish, and nuts, and avoiding excess salt, caffeine, and restricted fats to avoid the development and further progression of glaucoma. Take timely steps to defeat glaucoma!
Did you like our Article?
Excited
0
Happy
0
Not Sure
0
Silly
0
- Glaucoma available from Cleveland clinic
- Glaucoma available from Mayo Clinic
- Schellack N, et al. SA Pharmaceutical Journal. 2015 Jan 1;82(5):18-22.
- Al Owaifeer AM, et al. Ophthalmology and therapy. 2018 Jun;7(1):19-31.
- Ramdas WD, et al. Acta ophthalmologica. 2018 Sep;96(6):550-6.
- Bussel II, et al. Therapeutic advances in chronic disease. 2014 Jul;5(4):188-94.
- Tseng VL, et al. Journal of Glaucoma. 2022 Jul 1;31(7):494-502.
- García-Medina JJ, et al. Arch. Soc. Esp. Oftalmol. 2014 Mar 1;89(3):89-91.
- 5 tips for living better with glaucoma available from Hopkins Medicine
Our team of experts frequently monitors developments in the health and wellness field, and we update our articles when new information becomes available.
Current Version
Aug, 01 2023
Written By
Dr. Stefanenko Irina Borisovna
Leave a Comment